When you are faced with a diagnosis of young adult cancer one of the first concerns….though, obviously after the concern of making you better….is fertility. Everyone has a different fertility after cancer story (or infertility story). This one is mine.
At the appointment where I was handed a packet of information explaining about of the chemotherapy drugs that I would receive and what each of their side effects on my body (both seen and unseen…yes my pee was sooo red after one of them), I was also told about how my treatments could take a few different paths. As my mother-in-law and my dad each perched on a chair, with my husband, the doctor, a fellow, and a nurse taking up additional chairs and standing room, I sat awkwardly on the exam bed in the center of the room.
I decided to be treated in St. Louis at Siteman Cancer Center (Barnes), even though I lived in Champaign, IL with its own cancer center, because Siteman had a clinical trial that could help me avoid radiation treatments while still curing my cancer. Radiation treatments come with a load of short term side effects and also have the double whammy of bringing on a whole host of long term side effects…including more aggressive cancers later on in my life. The main premise of my clinical trial was that I would start with a regimen of ABVD (each letter standing for a different drug that was pushed or dripped through my IV each treatment session) for half of the prescribed treatment time. ABVD does not result in infertility any more than the average rate of infertility in the US population of young women. After this time, I would go through a set of imaging scans to asses the decline (or lack thereof) of my disease. If the ABVD was not successfully treating my cancer, than I would be switched to a different type of chemotherapy (BEACOPP…once again each letter standing for each different medicine) which most certainly would result in infertility. Following the BEACOPP, I would do radiation treatments. However, if the imaging scans showed that my cancer was responding favorably to the ABVD (meaning, the tumors were becoming smaller or disappearing entirely), then I would continue on with the ABVD for the rest of my treatments and would not receive the radiation treatments following chemotherapy.
Simple enough….but only kind of.
This all meant that before starting treatment, I didn’t know whether the chemo would result in infertility or not. It meant that I didn’t know whether I should prepare for infertility or not. It also meant that if I did want to prepare for infertility, I would need to do so before starting any of the cancer treatments. I had to decide whether dealing with a future possibility of infertility was worth allowing my cancer to continue spreading throughout my body. There were a million questions running through my mind… The main one was…Would waiting to start treatment make my cancer harder to treat (and therefore increase the risk that I’d need the harsher chemo)?
My husband (then fiancé) and I decided to meet with a fertility specialist. There we learned all about in vitro fertilization and the other various options that we had. I found this meeting to be much more emotional that I had expected. For a man, freezing sperm is a fairly straight forward process. For a woman, you can either choose to freeze eggs or to freeze zygotes (fertilized eggs). Freezing eggs doesn’t attach you to your current partner should you want to conceive with someone else but it also isn’t as successful as freezing zygotes. If you’re interested in more info on the various methods of saving fertility you can read more here. A big problem with these fertility saving treatments? I wasn’t infertile yet! Which meant that I didn’t have a diagnosis of infertility yet…which means that all of these fertility saving options can be quite expensive. If you’re looking into it, make sure you ask insurance how much they will cover and then ask around about how else you can receive financial assistance.
In the end, we decided to not delay my treatments. At the time, we felt comfortable adopting children if we needed to or even using a surrogate.
At the end of my treatments, the doctor met with us following an official round of scans showing that I was in remission. (WOOT!) After talking with us about what the next 5 years would be like in terms of follow up appointments and scans, she also talked to us about pregnancy. A reoccurrence of my type of cancer is much more likely within the first 3 years following treatment and we were strongly advised to not become pregnant during this time. The oncologist looked almost relieved that we weren’t bothered by this at all.
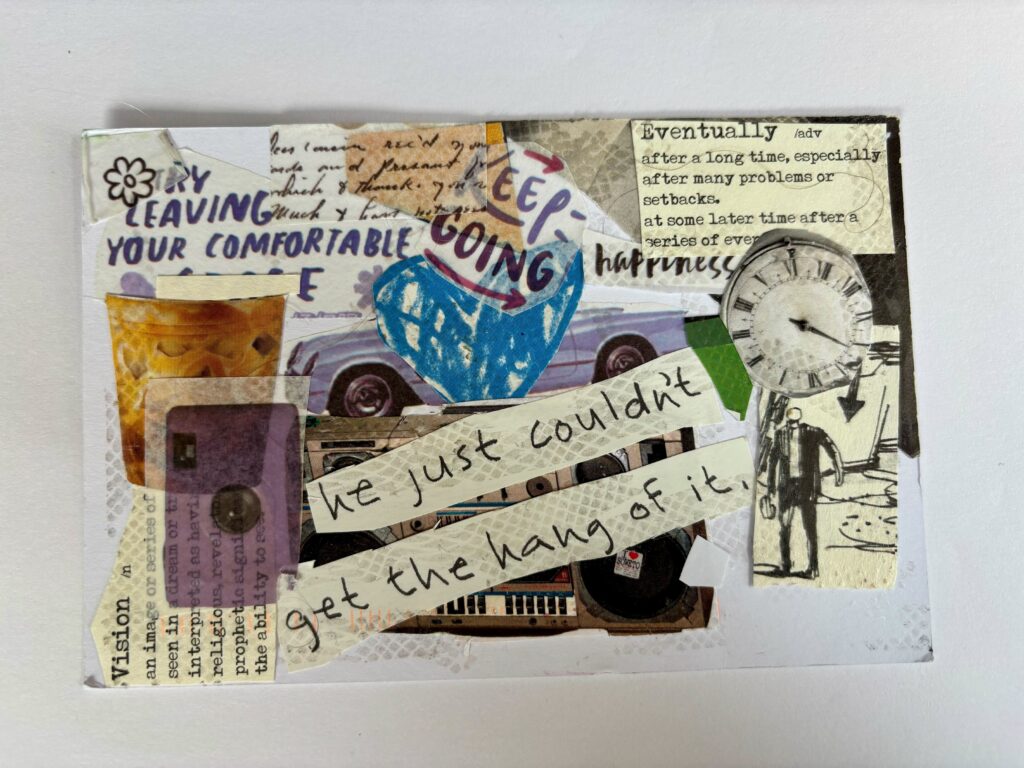
Now I am 3 years post treatment. I am 28 years old and my husband and I have been living on the assumption that we will probably start having a family in 3-5 years. Recently though, I watched this webinar on Sexual Wellness post-cancer (which is a bit boring but has a lot of info in it) and started to freak out. Why? You ask. Well, in the video, they mention (a little too off-handedly in my opinion) that women who undergo chemotherapy for breast cancer often experience ovarian aging of up to 10 years…meaning their ovaries now think they are 10 years older (and therefore perform like they are 10 years older). While I did not have breast cancer, one of the drugs that I received is shared by the two treatment regimens so I decided to look further into it. I spent a few days stressing over the fact that my 3-5 year window that I thought I had to start having kids before I was in an age bracket considered higher in risk, might now be extremely compromised.
I played phone tag a bit with the nurse who works with my oncologist. For about a week, I tearfully told just a handful of people how stressed and frightened this was making me…about how badly I wanted children and how my “I have a couple of years” plan was threatening to collapse. I eventually talked with the nurse but she didn’t have a lot to tell me. She explained that the chemotherapy treatments that I received tend to be less harmful to fertility than the one’s experienced by breast cancer patients but that she couldn’t tell me what my ovarian age was. She just said that she didn’t know how long we had been planning on waiting…but that if we wanted to start trying now, the oncology team (and my clinical trial) would be ok with it.
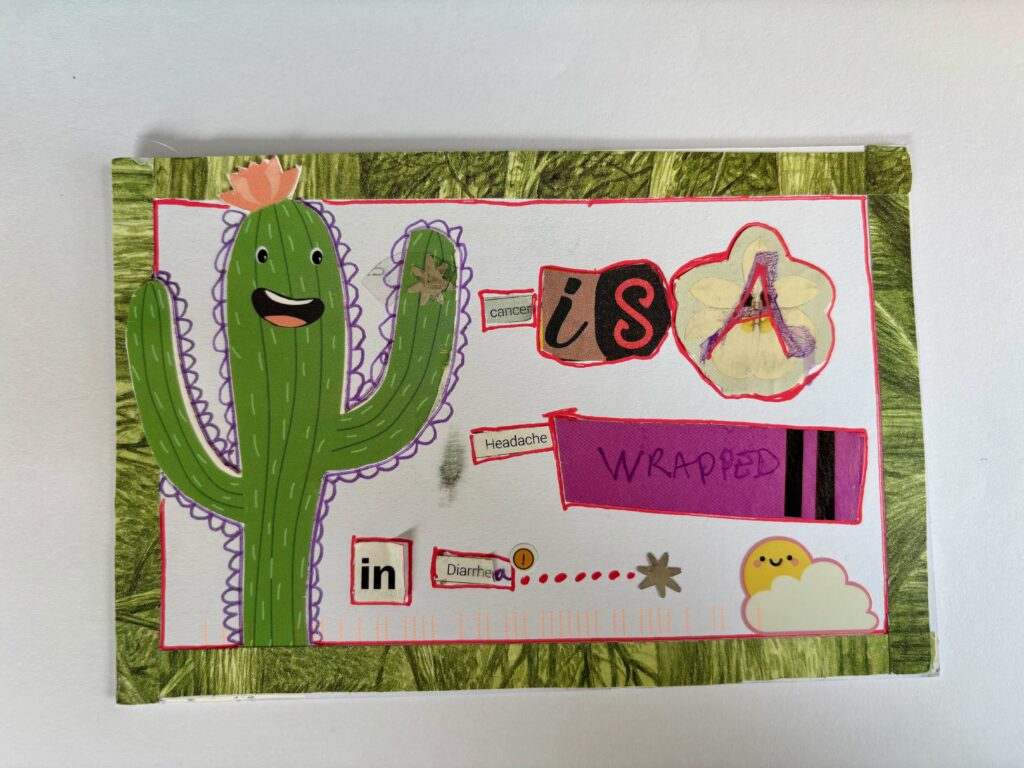
Thinking about our future, with kids, without kids, and/or adopting kids is stressful. Worrying about my fertility after cancer is stressful. Thinking about being healthy enough to have kids is stressful. Realizing that one.more.thing might be outside of my control is even more stressful. Cancer has done so much to me and to my family and I’m ready for its control to end.
This isn’t reality though. Cancer is part of my journey and whether or not I have my own children is also something I will just have to experience as it comes.
What has been your fertility after cancer story? What have you learned?
P.S. For a whole lot more information, visit the Fertile Hope website. If you are going through something similar, here are a few questions you should keep in mind when talking to your doctor.