After Facing Testicular Cancer, I Realized I Was Feeling Depressed – So I Asked For Antidepressants
Around the five month mark post chemo, I realized something was not quite right. It wasn’t my new fascination with discussing balls at every opportunity; it was more than that – my mood was not what it should have been. At first, I thought it was just the stress of returning to work and transitioning back to being a normal person instead of a cancer patient.
Upon closer inspection, I realized I was still feeling down, but it was summer, so the job reason didn’t make sense. If you’re not at regular reader of ABSOT, I am a teacher, and teachers don’t work in the summer – that’s the main reason we chose this, duh. (If you’re my principal and you’re reading this, please understand that this is a joke.)
However, a new school year began, and I noticed that I was feeling off and just not as enthusiastic as I once was about teaching. It wasn’t that I hated my job. I felt like something internally wasn’t quite right.
It was having an impact on my ability to teach to the best of my abilities.
My students were still learning, growing, and seemingly enjoying themselves, so they didn’t appear to notice my internal struggle. Nor did my administrators, who are awesome and amazingly supportive of me, or my co-workers, who are also pretty great and put up with endless ball puns during team meetings. Regrettably, we don’t teach about spheres during the geometry unit.
In addition to feeling slightly off at work, I also realized I was feeling irritable and was much quicker to get angry at home. In October, I experienced a full on panic attack while watching an episode of Stranger Things on Netflix on the eve of my orchiectomyversary. Overall, hobbies like reading and cooking didn’t bring me as much pleasure as they once did, and I just felt generally pretty flat.
My past experience with depression
As I’ve alluded to numerous times through my writing on ABSOT, I battled with depression in high school. However, since my only job at that point in my life was to be a student (and school had never been a struggle for me, since I was in the gifted program), it didn’t have an impact on my “job.” It dawned on me that I was now feeling some of the same effects I did back them.
Knowing that having depression at a young age puts me at risk for a recurrence later in life, I decided to look into research about cancer survivors and PTSD/depression to fully understand just how stacked the cards were against me. It didn’t bode well when I first typed “cancer survivors and…” into Google, and “PTSD” and “depression” popped up as the first two suggested results (followed by “alcohol”).
As I researched more, I found this study from 2017 that said about 20% of cancer survivors experience PTSD symptoms within six months of diagnosis. The CDC also reports that cancer survivors take anxiety and depression medication at almost twice the rate of the general population.
After finding this information, I decided to ask for help, specifically in the form of antidepressants at my follow up visit in December. Dr. Maurer agreed to prescribe them, and I thought it would be all pretty rainbows and fluffy unicorns immediately.
Did the antidepressants help right away?
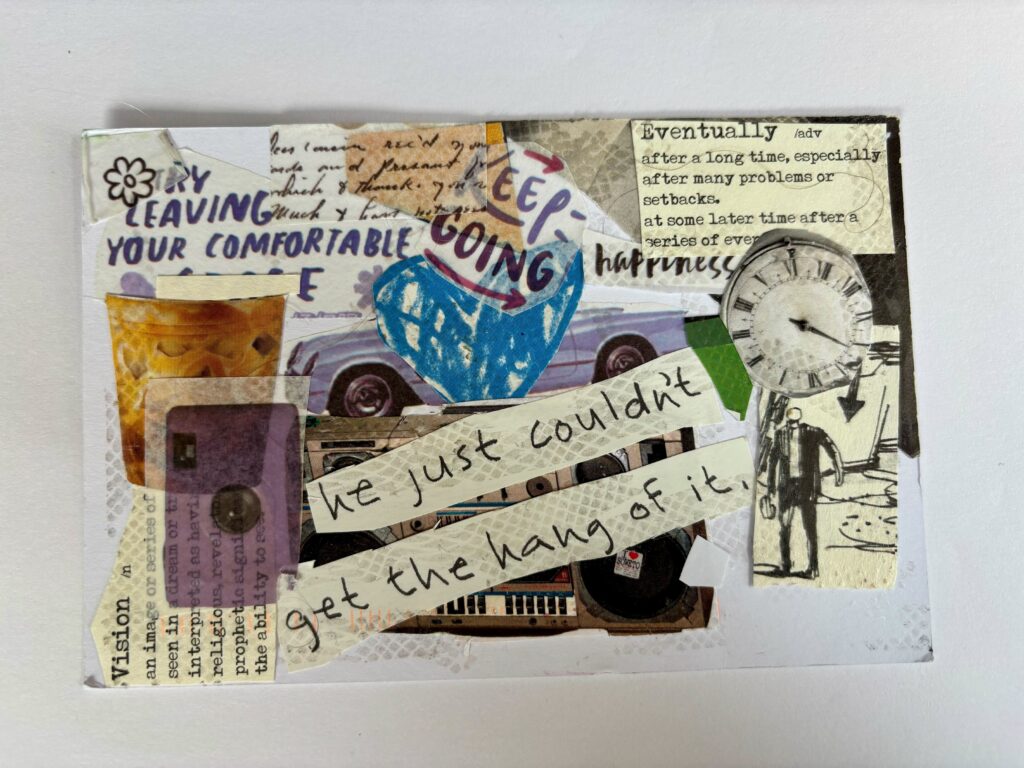
However, about four weeks later, I felt no different. I knew antidepressants could take up to six weeks to show major changes, but I wasn’t feeling even slightly better. Perhaps I even felt worse, as I had these “happy pills” and I still felt down. Maybe something was just wrong with me – beyond the missing testicle.
I’ve learned to be open with my health and feelings, so at my med check up with NP Sullivan, I basically said, “Hey, I don’t think these are working.” Since I am obviously super medically qualified (read as: not qualified at all), I supported my theorem by saying I was on the same dosage I was in high school, and High School Justin was about fifty pounds lighter and ten years younger (and had a terrible taste in hairstyles and girls, but that’s a different story for another day).
NP Sullivan actually agreed with me and decided to increase my dosage. I wish I could say that this was the end of my frustration, but it wasn’t.
Insurance doesn’t treat depression as a serious matter
However, this new struggle wasn’t internal – it was externally driven towards insurance companies and American healthcare in general. If you’re an international reader (and I know you’re out there, since according to Blogger’s data I have readers on every continent, except Antarctica, which is a shame since it’s cold as ball(s) there), appreciate it if you have a better healthcare system.
When Dr. Maurer first prescribed the pills in December, my prescription was denied, since the pharmacy needed to get “pre-authorization” because apparently, a doctor’s orders aren’t enough. This wouldn’t have been a huge deal, but I was going out of town for a week and wanted to start the pills immediately. Out of desperation, I ended up paying out of pocket for that first fill. About two weeks after starting the pills, the pre-authorization came through, just in time for my dosage increase.
And just in time for another claim denial. Apparently, my original pre-auth covered me only for the original dose. The fact that insurance claims can be denied through an automated system by non-medical professionals is ridiculous to me. Insurance companies, do better.
Long story short, the insurance claim handlers at Dr. Maurer’s office are awesome, and I got pre-authorized for the new dose. (Maybe my mini-rant on Instagram story helped too!) This new pre-auth lasts for a year, and hopefully, I won’t need any more increases.
The positive impact from the antidepressants
To be honest, I don’t think I will need it. I’m not really sure when I noticed that I was feeling better, but when I wrote my “12 Months Later” post in late-January, things were definitely looking up. I was getting more into the swing of lesson planning and teaching, minor things didn’t bother me as much, and I didn’t find myself complaining as often. I wish I could say that colors were suddenly more vivid, but I’m colorblind and colors don’t ever look bright.
It’s now the end of February, and I feel so much better than I did in September. (Side note – I really feel like Christopher Nolan with the amount of time jumps in this post. My bad.) While I would never say I hated work, I definitely have a better attitude when I walk through the doors of Room 31. Exercise, writing, reading, and cooking have become more enjoyable again. I’ve even developed a new hobby – Speed solving of Rubik’s Cubes. I know, I am super cool and not nerdy at all.
While writing this post, I realized that this one has a better feel and tone, as compared to some of the posts I wrote between September to January, even though it’s about depression, I feel more like myself on a day-to-day basis. I haven’t resumed any sort of formal therapy program, but I know that is definitely recommended while on these pills. It’s on my to-do list to look into in the future.
My takeaways – and how we can treat depression better
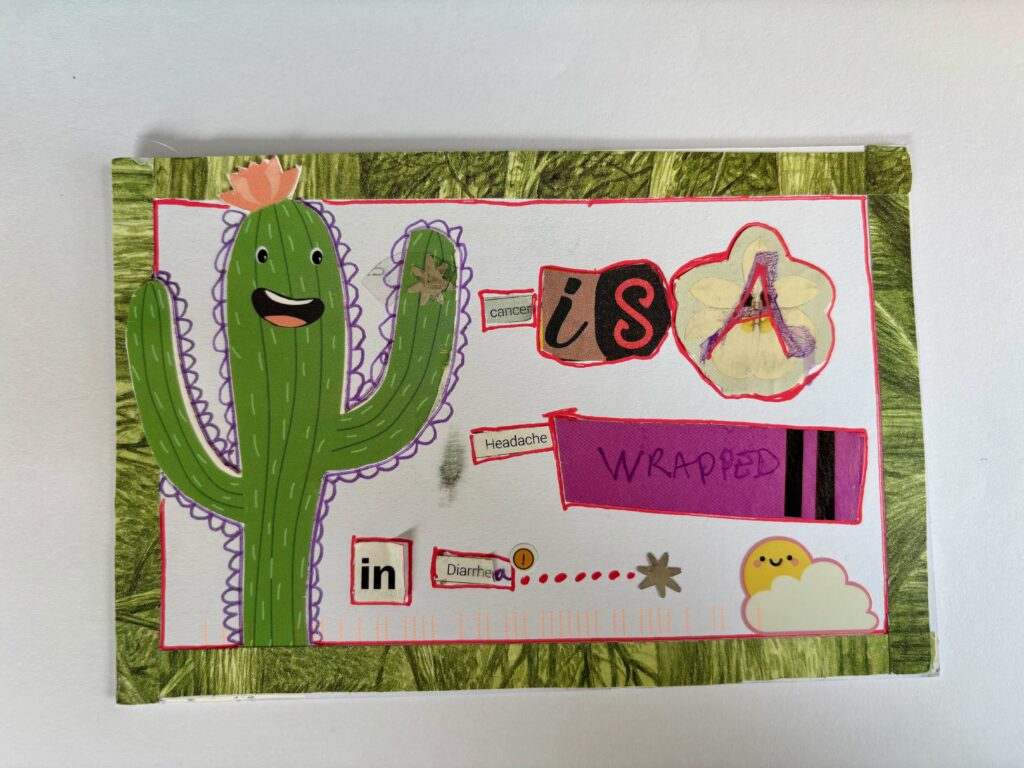
My biggest takeaway from this all is to ask for help if you feel you need it. There seems to be such a stigma around mental health and this post is an effort to be open and transparent to help dispel it. Sometimes, mental health isn’t even viewed as a necessary thing to take care of or treat as a serious matter. We treat our bodies and help them to heal when we are sick or injured; why should our mental health and brains be different?
The debacle with the insurance company and preauthorization helps to underscore this issue. When I had “probable strep” in January, although the test came back negative, the company had no problem approving amoxicillin, even though it probably wasn’t necessary. Any other prescription for my myriad of side effects during chemo was filled without an issue. But needing antidepressants? I had to jump through hoops to get those.
I recently saw a Tweet that said, “Depressed people don’t need Prozac. They need running shoes and fresh air.”
That’s a damaging narrative.
I tried that, and continue to exercise, but it wasn’t that simple for me. If that’s your opinion, fine. Go run or whatever else works for you. But don’t shame other people for trying what might work for them. Just as I’m not going to fault you for trying homeopathic medicine, don’t go throwing crystals at me for what I’ve chosen. Positive thinking just isn’t enough sometimes.
I hope that this dosage continues to keep my mood elevated and on the upswing. I have no idea how long I’ll need to be on the antidepressants, but I’m not worried about it. What matters to me is that my emotional healing is beginning to catch up to my physical healing, the disparity between the two being something that has been nagging at me since I was cleared for remission.
However, this is something that I should have seen coming. They removed half of my “lower brain” and left my upper brain fully intact… no wonder it’s taking twice as long to heal!
This piece was written by Justin Birckbichler and originally posted on his blog, A Ballsy Sense of Tumor.